Jurisdiction:
Taiwan
Organ System:
Head and Neck
Funding Organization:
- Service Platform of Molecular Medicine Research Center, Chang Gung University, Taiwan
Research Organizations:
- Chang Gung University, Taiwan
- Chang Gung Memorial Hospital, Taiwan
- New Taipei Municipal City TuCheng Hospital, Taiwan
- National Cancer Institute, USA
Principal Investigators
:- Yu-Sun Chang
- Jau-Song Yu
- Kai-Ping Chang
Publication:
External Links:
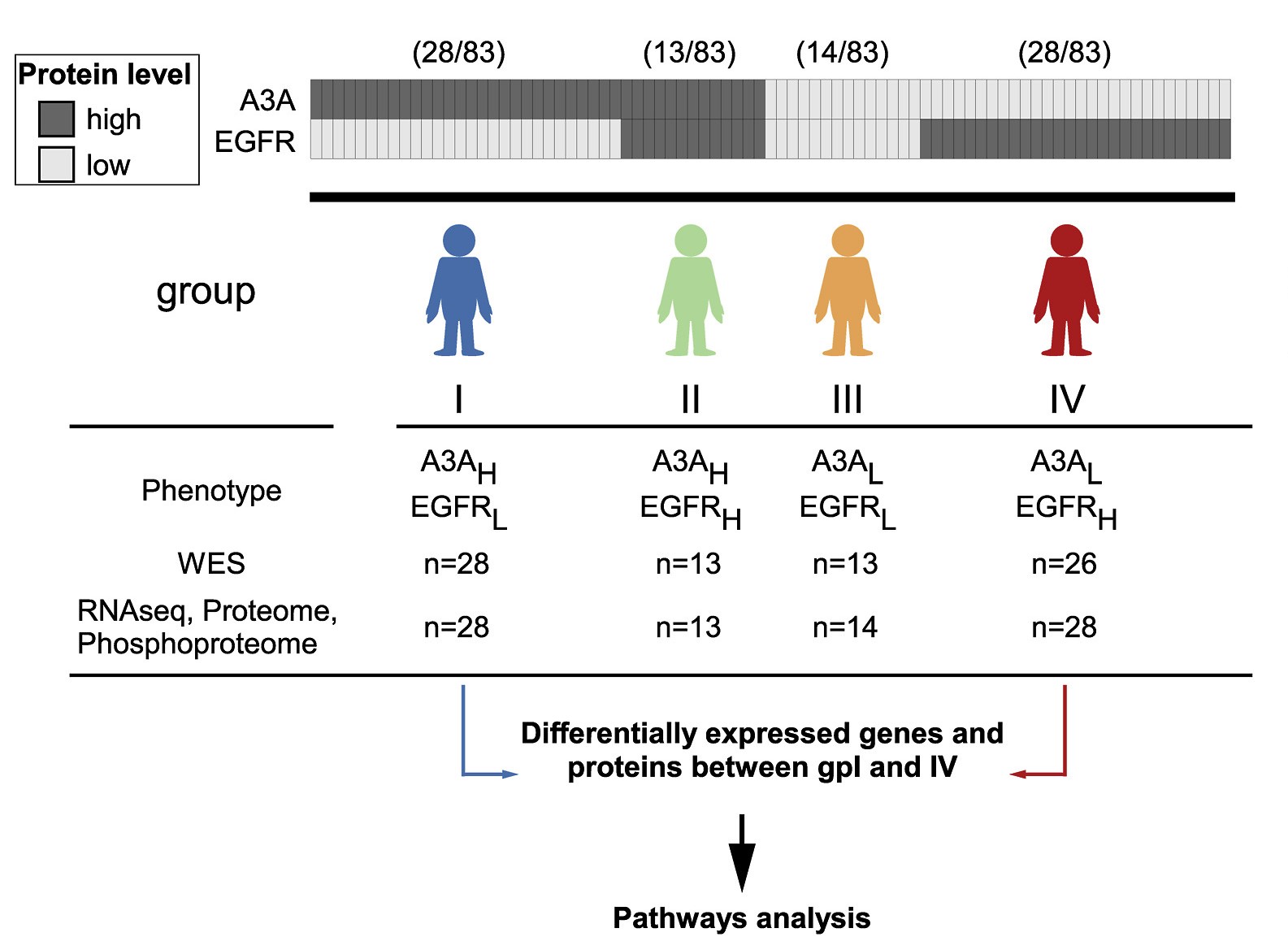
Oral cavity squamous cell carcinoma (OSCC), a leading subtype of head and neck cancer, exhibits high global incidence and mortality rates. Despite advancements in surgery and radiochemotherapy, approximately one-third of patients experience relapse. To improve current targeted and immunotherapy strategies for recurrent OSCC, we conducted multi-omics analyses on pretreatment OSCC samples (cohorts 1 and 2, n = 137) and identified A3A and EGFR, both at the RNA and protein levels, as inversely expressed markers for patient stratification and response prediction. Survival analysis demonstrated that elevated A3A or PD-L1 expression levels correlated to improved responses to anti-PD-1 therapy in patients (cohort 3a, n = 50, IHC). In contrast, high RRAS expression (cohort 4, n = 252, qRT-PCR) was significantly associated with OSCC recurrence. Cell-based experiments revealed that RRAS was involved in radiotherapy and cisplatin resistance through the EGFR/RRAS/AKT/ERK signaling pathway. In OSCC patient-derived xenograft (PDX) mouse models, treatments with cisplatin and cetuximab (anti-EGFR) effectively reduced tumor size in EGFR-high-derived (#34) but not A3A-high-derived (#22) PDX tumors. Our study demonstrated that A3A-high tumors were immune-hot and responsive to anti-PD-1 therapy, whereas EGFR-high tumors exhibited chr.7p11.2 gains and DNA repair alterations. Additionally, RRAS-high tumors were associated with OSCC recurrence via AKT and ERK phosphorylation and demonstrate improved clinical outcomes with cetuximab therapy (cohort 3b, n = 49, IHC). This study emphasizes the significance of A3A and EGFR expression levels in OSCC patient stratification and precision therapy, suggesting the use of anti-PD-1 or anti-EGFR treatments, respectively based on these biomarkers. Furthermore, RRAS emerges as a novel prognostic marker for local recurrence.